If cancer is the emperor of the entire maladies, definitely depression is the king of mental illnesses. However, what precisely is depression? And what are the determinants of depression? Although up till now the overwhelming majority of research has searched for the roots of depression in the mind and the brain, new innovative studies are showing how depression is not only a mental illness; however, a bodily one as well. Also, the immune system is a vital association here.
These book chapters examine some of the newest science to describe how the immune system makes use of inflammation to combat disease, the reason why this can negatively impact our emotion and action, and how the inflammation hypothesis could develop revolutionarily new, holistic cures of depression.

Chapter 1 – Physical sickness can make you become depressed, and this could be caused by inflammation.
Have you ever had a really bad cold that made you strangely sad, tired and antisocial?
When you fall sick, it’s okay to feel slightly depressed. As a matter of fact, it reasonable for you to feel like this, in order to remain in bed and keep your energy for fighting off the infection. This is done by your immune system by triggering inflammation in your entire body that’s intended to end the cold virus. As soon as the virus vanishes and the inflammation lessens, your mood rises again.
However, there might be further aspects of the process of cold-induced gloominess than we assumed. An increasing number of scientists are claiming that it could offer a significant hint to knowing depression.
They assume that gloominess is not produced by the illness itself or your negative feelings about being ill; however by your immune system’s response to the illness: extensive bodily inflammation. Also, these scientists are beginning to suspect that persisting inflammation could be the reason for the long-term mood disorder we usually refer to as “depression.”
A story about a drug for rheumatoid arthritis shows the strong impact that inflammation can have on our mood.
Rheumatoid arthritis is an autoimmune disease of the joints that cause them to progressively stiff and swell up. In autoimmune diseases, the immune system brings about a pointless, chronic inflammation in reaction to some of the body’s components or parts–which are the joints in this situation.

During the 1990s, scientists eventually discovered an antibody against one of the vital inflammatory proteins of the disease. They created a drug with this antibody that would assist minimize the inflammation, and hence relieve the painful side effects of stiffness and swelling.
In the year 1999, the first kind of that drug was brought to market under the brand name Remicade. To a lot of rheumatic patients, Remicade seemed like a miracle treatment. Given as an infusion, it didn’t only provide instant relief of pain; however, it made the patients feel happy immediately and cheerful as well. At the University College Hospital in London, the patients’ ecstatic “Remicade high” made nurses fight over who had to give the infusion.
Although not really studied, this Remicade high proposes that decreasing inflammation can enhance people’s moods. On the other hand, it looks as if a lot of inflammation can make people feel depressed. For us to know the reason why this might be, let’s take a closer glance at how inflammation functions.
Chapter 2 – Inflammation is a normal response of our immune system to defend us from infection.
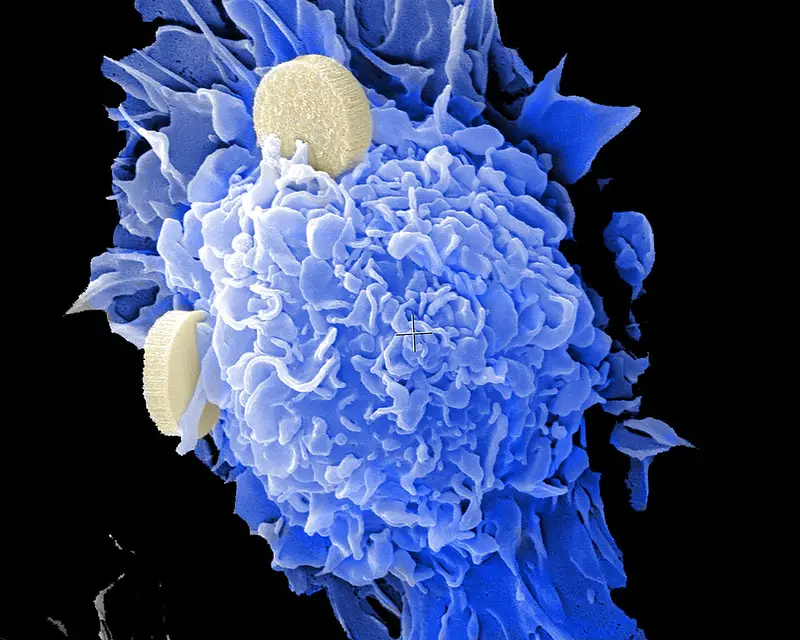
Human beings have been at war since the start of time. With each other usually enough; however, also against the thousands of little non-human attackers that swarm our bodies regularly. The immune system doesn’t just trigger when we have a cold. Day and night, our immune systems protect us against aggressive viruses, worms, pathogens, bacteria, germs, and bugs – jointly known as antigens – which could otherwise bring about to severe sickness or death.
The human immune system is made up of several parts and components. Its most vital soldiers are white blood cells, which can be broken down into different kinds of specialized immune cells like macrophages, and lymphocytes.
Macrophages are huge consuming cells whose work it is to kill dangerous antigens by enclosing them in a membrane of digestive enzymes. They are located in various places all through the body and are particularly many in sensitive parts that usually get in touch with things from the outside, like your urinary tract, eyes, lungs, and gut.
Macrophages have been taught over thousands of years of evolution to detect different types of harmful particles. As soon as a macrophage has detected and consumed that kind of particle, it moves to the closes lymph node, which is glands found in your neck, armpits or groin. In that place, it shares the information it has learned about the invader with other cells – the lymphocytes.
The information about the infectious particle lets the lymphocytes to coordinate the body’s immune reaction. If the threat is severe, lymphocytes will release antibodies that move through the blood and bind to the dangerous antigens. This, eventually, assists other macrophages to detect the attackers more easily and immediately damages them.
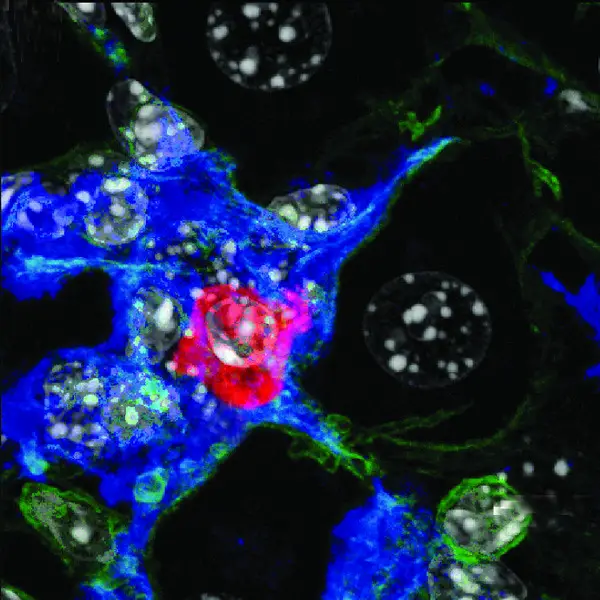
Macrophages communicate information to one other as well through cytokines, proteins which arouse other macrophages to be more moveable and hostile. Unluckily, their blind fury as they attempt to look for and digest the dangerous attacker can lead to collateral damage to our nerve and muscle tissue. This is the reason why heavy inflammation is usually accompanied by redness, stiffness, and pain in the affected regions. Also, increases in both blood flow and fluid retention make it swell too.
Inflammation can be acute, for instance when you have a cut or a wound. However, inflammation can also turn into a chronic condition. In chronic inflammation, your cytokines, lymphocytes, and macrophages, are permanently moderately triggered, and their activities lead to the destruction of the surrounding tissue and hinder your body’s normal work.
Chapter 3 – The principle of Cartesian dualism has kept contemporary medicine from examining the connections between mind and body.
During the author’s early training as a physician, he treated an elderly lady for her rheumatoid arthritis. Since the woman looked really depressed, he asked her about her mood and social life during the examination. During that time, he didn’t suspect that the inflammation underlying her arthritis could also trigger her depression –however, he felt it was significant to fix her entire problems holistically.
After the examination, the supervisor of the author harshly told him that his duty was to treat the lady’s arthritis and not her depression. Nevertheless, anybody with that kind of a terrible disease would most likely be a bit depressed.
Even nowadays, medicine puts a limit on physical and mental health issues. Physicians hardly question their patients about mental symptoms, whereas therapists and psychiatrists rarely think of the underlying physical problems.
One man is to be blamed for this. René Descartes was a well-known seventeenth-century mathematician and philosopher who suggested that humans are separated in two. He suggested that the human body is just like a machine that functions in relation to physical laws, whereas the human mind, or “soul”, is an irrelevant spirit that can’t be examined with scientific approaches. Descartes believed that the soul came in touch with and regulated the body via the pineal gland, a little bulbous structure found at the lower part of the brain.
Now, we are aware that this is incorrect: the pineal gland is a very basic brain structure that works as our biological clock, controlling our day-to-day and seasonal cycles.
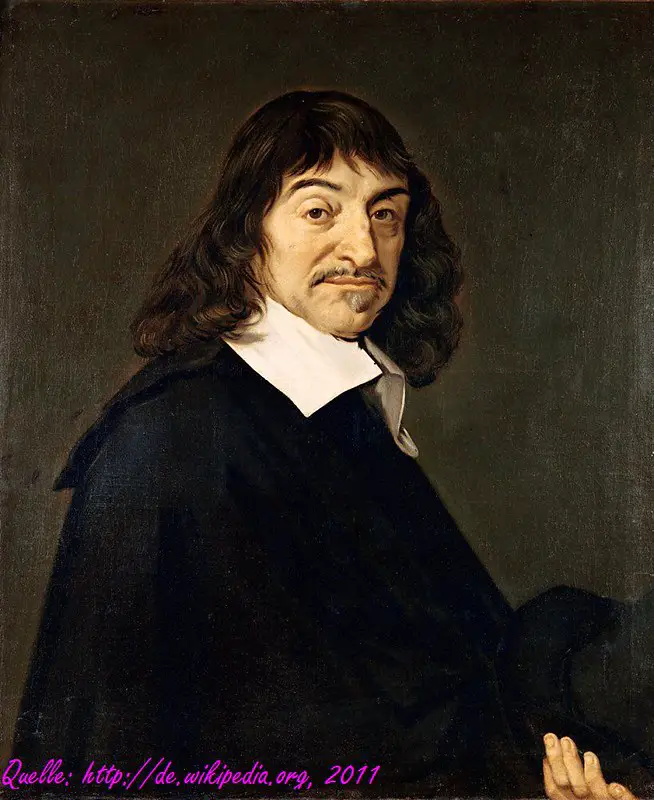
However, Cartesian dualism controlled medicine for centuries, as scientists concentrated only on controlling and measuring the body, whereas the mind stayed strange and unreachable. It was just during the nineteenth century that the mind started to be seen as a topic deserving of extreme scientific study.
Sigmund Freud, the father of modern psychology, created the discipline of psychoanalysis to direct this systematic inquiry into the human psyche. However, the threat of Cartesianism haunted him as well. At the start of his career, Freud wished to study our mysterious minds as well as our physical brains, holistically. However, after having a disagreement with his mentor over this absurd, anti-dualist idea, Freud moved away from this outlook, and the discipline of psychoanalysis came to target the mind as its own individual entity.
During the twentieth century, scientists eventually started exposing the links between the mind and brain. However, even as the field of neuroscience turned into its own reputable discipline, they usually ended up treating the head as though it was different from the remaining of the body — and the effect of this idea can still be felt up till now.
Chapter 4 – Ever since the creation of Prozac during the 90s, there have been no key innovations in the treatment of depression.
If you’re an ironclad Cartesian dualist, the idea that you can treat the mind by altering chemicals in the brain is unimaginable.
However, nowadays, antidepressant medicines that assert to balance the chemical makeup of the brain have become one of the few treatment choices for depression.
Just like a lot of medicines for mental illness, they were found mistakenly. Immediately after World War II ended, scientists discovered that the molecule iproniazid, gotten from rocket fuel utilized by German forces, put an end to the procreation of harmful Mycobacterium tuberculosis bacteria. During those days, lung disease Tuberculosis, or TB, was one of the main causes of death.
In the year 1952, when the new drug called iproniazid was tested at one of the numerous TB sanatoriums in the US, it was a miraculous accomplishment. It didn’t only kill the TB bacteria in a situation of weeks, it instantly made patients more happy, active and social. Nurses stated that patients that were formerly bedridden were dancing in the wards.
A few years after, scientists discovered that iproniazid didn’t just kill TB bacteria, however, it enhanced specific neurotransmitters as well – which are chemical molecules that the brain’s 100 billion nerve cells make use of to communicate with one another.
To describe the reason why this had an antidepressant impact on patients, scientists spread the theory that depression is a result of an imbalance of neurotransmitters in the brain.
According to this theory, Eli Lilly the US pharma company created a new group of antidepressants enhancing the levels of the neurotransmitter serotonin, named Selective Serotonin Reuptake Inhibitors, or SSRIs in short.
During the year 1987, the first SSRI was brought to market under the currently-iconic brand name Prozac. In the year 1995, it had made $2 billion in sales across the world. As Prozac, research for new antidepressant medicines has failed. The drugs that have come after are simply different forms of the same thing.

The issue is, although SSRIs look to work for certain people, the serotonin theory of depression is not really convincing. Up till now, there is no research that has been able to verify that people that are depressed really have lesser levels of serotonin than others. The same applies to any other neurotransmitter.
This signifies that the only slightly drug treatment that is effective for depression available nowadays is not much more than the outcome of a fortunate stab in the dark. Then, it is not a surprise, that science has made no significant progress in drug treatments for depression in 30 years – it still hasn’t discovered the accurate target.
Chapter 5 – New areas of medical research are discovering promising connections between inflammation and depression.
During the 1990s, around the period that Prozac was launched, the first articles associating depression to the immune system were published in complex medical journals. They comprised of headings like The Macrophage Theory of Depression (1991) and Evidence for an Immune Response in Major Depression (1995). In understanding the event, these theories look like a huge discovery. However, during that time, they were mostly disregarded – they were not suitable for the new serotonin story.
However, these papers initiated the start of two new medical areas of research: neuroimmunology, which examines the association between the immune system and the brain; and immunopsychiatry, which concentrates on the link between the immune system and mental health.
Since that time, various studies have shown the association between depressive tendencies and higher levels of specific biomarkers – specifically, inflammation proteins called cytokines and C-reactive protein (CRP). A Danish study that was conducted, which comprised of more than 70,000 members of the overall public and ended in 2014, revealed that the more the levels of CRP in someone’s blood, the more prone they were to have negative, self-critical feelings.
However, in order to reveal that inflammation brings about depression, we have to verify that it occurs first, before the depression. Current studies have done precisely this. In the year 2014, long term research of 15,000 British children revealed that the children who were a bit inflamed at nine years of age were one and a half times very likely to experience depression at the age of 18.

The study of the effects of vaccination is a different method to test the inflammation hypothesis. When you receive a vaccine against a certain disease, your doctor is actually administering you with a weakened form of the disease’s antigen, in order for your immune system to form antibodies against it. This generates a temporary inflammatory response that usually has an instant effect on people’s feelings and actions.
In one research a typhoid vaccination was administered 20 healthy young people, increasing their levels of inflammatory cytokines for a short time. Afterward, when images of sad faces were shown to them, their brain scans revealed heightened activation of their emotional brain connecting, something normally seen in people that are depressed.
However, how is it likely that an old defense mechanism of the human body influences mood in such an extreme manner? In the following chapter, we’ll examine the links between the immune system and the brain.
Chapter 6 – Inflammation in the body can lead to an inflammatory response in the brain that has an effect on our mood and action.
Only in the few past decades, scientists thought that it was almost not possible for the immune system to have an effect on our brain. They believed that the brain had its own, totally different immune system, protected from the remaining of the body by the alleged Blood-Brain Barrier, or BBB. The BBB is a thick wall of cells that surrounds the brain and stops molecules circulating in the blood from going straight through to the brain.
However, in current years, scientists have found out that the BBB isn’t as impermeable as formerly believed. Not just are there openings between the BBB cells that let specific molecules and proteins to go into the brain; the cells themselves can react to inflammatory signs of the body, and transfer that information to the brain.
For instance, when inflammatory cytokines in the body get to a specific threshold, a specialized nerve known as the vagus nerve transfers a signal to the brain that starts its own inflammatory reaction. Due to that, macrophages in the brain called the microglia, get more “angry” and active and begin to produce cytokines themselves.
Similar to the macrophages in the remaining of the body, this activity can lead to the collateral damage of the surrounding cells, damaging the links between them, reducing their communication or completely killing them off. This nerve destruction could be a likely reason for the memory loss and cognitive impairments related to chronic inflammation.
Also, Inflammation in the brain interrupts the flow of neurotransmitters. For instance, Serotonin is produced by nerve cells from the base protein known as tryptophan. However, inflammatory cytokines inspire nerve cells to make use of tryptophan to form other kinds of proteins such as kynurenine instead, which aid the process of inflammation; however, they are dangerous to nerve cells in the long term.

Furthermore, by reducing its fundamental building material, kynurenine potentially reduces the levels of serotonin in the brain. This eventually could have an effect on our mood, appetite, and sleep, and might as well explain the reason why some extremely inflamed patients do not really react well to SSRIs.
Therefore, different from what scientists assumed for decades, chronic or heavy inflammation of the body can cause inflammation of the brain easily. However, the brain as well works on the immune system. Inflammation in the body can be hindered by transferring an electrical signal back via the vagus nerve to the immune system control center of the spleen.
Chapter 7 – Chronic inflammation can be a result of stress, age, obesity, and autoimmune disorders.
Up till now, we’ve understood that inflammation is a normal reaction of the immune system; however, when it becomes chronic it leads to severe collateral damage to our bodies and brains. This, eventually, has an impact on our moods, thoughts, and behavior.
However, what leads to chronic inflammation?
Autoimmune disorders such as lupus, rheumatoid arthritis, and Hashimoto’s disease are likely causes of persistent inflammation. In current years, a lot of formerly misunderstood illnesses have been discovered as autoimmune diseases, triggered by the body’s damaged immune reactions to some of its own building blocks.
For example, when the immune system starts to turn on the cells in the pancreas that release insulin and the body loses control over glucose levels, this causes diabetes. Just like a lot of other autoimmune disorders that lead to chronic inflammation, diabetes is usually associated with depression.
However, even supposedly “healthy” people can experience chronic inflammation caused bu genetics, and specific conditions and lifestyle decisions. For every one of us, levels of inflammatory cytokines and CRP naturally rise as we age. Also, inflammation has been demonstrated to be naturally greater in the winter months – most likely due to all the flu and cold viruses happening around during that time of year.
Another risk factor for inflammation is obesity. Nearly 60% of the cells in fat tissue consist of macrophages and people that are overweight have greater levels of cytokines and CRP. This may as well be a cause for higher rates of depression in people that are overweight.
However, maybe the largest factor to chronic inflammation of all is stress, which is as well the best understood, still least know, cause of depression. 80% of depressive episodes are preceded by a stressful situation like the death of a loved one.
At the moment, scientists now understand that stress, meaning our body’s acute or chronic reaction to social or physical threats, also has an effect on the immune system. Levels of cytokines and CRP are greater in people that are going through severely stressful conditions like poverty, debt or social isolation. However, even small social stresses like public speaking can trigger temporary inflammatory.
In a study that was conducted, scientists checked participants’ cytokine levels and then they asked the participants to talk to an audience of four people for 12 minutes, followed by the audience questioning the participants’ about math questions. After the task, when the scientists checked cytokine levels once again, they were extremely higher – the stress of public questioning had made the participants become temporarily inflamed.
Chapter 8 – A sensitivity to inflammation as well as depression could have assisted our forefathers to live.
Now that you’ve known about how inflammation can lead to depression, you most likely want to understand the reason why this is so.
When we ask the question on the reason why our bodies and brains do this or that, the reply will typically be natural selection. If we stick to Darwin’s evolutionary theory, then one way or another, at some point in human evolution, inflammation and depression definitely have assisted the human species to live.
This looks like a paradox, considering the fact that depression reduces about ten years from the average life expectancy. However, a lot of human characters are old, and although they may have assisted our ancestors to live so long to procreate and transfer their genes, they are pointless or even unfavorable to us in the contemporary era.
According to the author, the most fascinating evolutionary theory of depression concentrates on the immune system. It dates back to 150,000 years ago to our earliest ancestors staying in the African savannah. During that time, life was risky, and infectious diseases acquired through childbirth, wounds or detrimental pathogens abounded.
This signified that gene mutations that enhanced inflammation –allowing macrophages to be more active and annoyed, heightening cytokine levels and boosting the body’s germ-killing power – would have made someone very likely to live.

However, the illness behaviors related to inflammation, which we would now identify as symptoms of depression, would have been beneficial as well. For one, lethargy and tiredness oblige the body to rest and save resources for defending one’s self against the infection. And social isolation could have been helpful for the tribe at large, as other people would have been unlikely to get the infectious disease. Hence, even if the person that is ill eventually dies, genetically related members would be very likely to live.
Infection usually occurred from injuries or wounds sustained during fighting. Anybody who spontaneously became inflamed in circumstances that could cause hostility would have a headstart in fighting it.
For instance, think of two of our forefathers fighting over a piece of meat. One of them has hereditary genes that trigger inflammation early, as a reaction to the social stress of fighting. Then, when the physical fight eventually happens, this forefather will be capable to fight off following infection of the injuries sustained in the fight faster and easily. This could be the reason why up till now, even trivial social stress, like public speaking, can lead to an inflammatory reaction in the body.
Chapter 9 – Medication and therapy that lessen inflammation, assure new hope for treating depression.
After reading these book chapters, If you suspect that your depression is a result of inflammation, you most likely desire to know what you can be done about it.
Unluckily, still, the professional treatment choices for inflammatory depression are scarce.
Your doctor could do a blood test for inflammatory biomarkers like CRP. If the levels of your CRP are more than 3 mg/L, this could possibly be an indication of chronic inflammation. However, except you have an existing physical sickness that is triggering the inflammation, like gum disease or IBS, your doctor won’t recommend any anti-inflammatory medication for you.
The reason is that anti-inflammatory medicines are not approved for the treatment of depression yet. Currently, there basically aren’t adequate studies to decisively verify that the effects of anti-inflammatory medications on depression are greater than their side effects, like thinning the blood or destroying the gut.
Also, the pharma industries aren’t essentially ready to create experimental new drugs. For several years, they have kept working hard at antidepressants that aim at serotonin as well as other neurotransmitters, without any new theories or aims to explore, and with few profitable outcomes. Due to that, they have moved away from the mental health subject.
According to the authors’ own experience in the field, he calculates that the first anti-inflammatory medications for depression will be available in the market in about five to ten years.
A faster way could be to repurpose anti-inflammatory medications used for other diseases. current studies have revealed that anti-inflammatory medications that cure rheumatoid arthritis, psoriasis and asthma have a slight antidepressant side effect on people that have depression that still exceeds the typical SSRI.
A different method that is already approved for the treatment of depression is the usage of bioelectric devices that arouse the vagus nerve through vibrations in the ear, to prevent inflammation. For a lot of people with depression, this treatment option certainly does look to work; however, it’s not really prevalent yet.

Your doctor is very likely to suggest therapy and lifestyle modifications that fight likely underlying determinants of inflammation, like stress and obesity. This could entail attempting yoga, meditation or psychotherapy; or altering the food you eat and exercising.
One thing that’s turn out to be progressively obvious is that there is no one-size-fits-all treatment for depression. Mental illness can be caused by so many factors, which is the reason why treatment has to be tailored and holistic, targeting to disrupt the vicious cycle of stress, inflammation, and depression. Knowing just how inflammation fits into the situation will be a significant step toward accomplishing this.
The Inflamed Mind: A Radical New Approach to Depression by Edward Bullmore Book Review
Since the emergence of Prozac during the 90s, there have been few improvements in our treatment and knowledge of depression. However, in the last few years, science has been discovering new connections between depression and inflammation triggered by our immune system. When inflammation turns into chronic as a result of autoimmune diseases, stress or other lifestyle issues, it can negatively impact our mood, feelings, and action. Anti-inflammatory medications and stress-reducing therapies assure a strong treatment choice for depression.
